Immunity, Lung Damage and COVID-19
Early on the pandemic the SARS-CoV-2 virus appeared to attack deeper parts of the airways leading to a massive compromise in blood-gas exchange. Everyone was rushing out to buy Arterial Oxygen monitors (pAO2) to monitor their status, and ICU’s were overwhelmed with patients needing ventilation. Whilst the pandemic is far from over, the new variants display greater infectivity (approaching that of measles now) but the ramifications seemed to have shifted towards upper respiratory issues. Lethality has been reduced as a result although in Long COVID the pathology can persist ( Lung Damage and Long COVID ) .
This begs many questions, but one aspect that I wish to detail is what was driving the pneumonia, the heavy lungs and poor gas exchange that typified the early hospitalizations? We are likely to be familiar with terms like “Cytokine Storm” and “Oxidative Stress” but how do they play a role? The hallmarks are similar to autoimmune diseases, which is where the immune system attacks oneself and tissue damage is a consequence of “friendly fire”.
Despite this knowledge, there was a massive call to augment and enhance immunity. Admirable concept but misguided in this case. While there is a need to clear the virus, the part of the immune system that typified the cytokine storm was actually a driver of lethality and morbidity. It is also plays a dominant role in LONG COVID, where dysfunction persists beyond the infection and compromises the quality of life.
In essence, the solution to the problem was not to enhance the immune system, but to dampen, suppress or rebalance the Th1 part of the immune system that is now out of control and causing rampant damage. Enhancing this part of immunity will not help, indeed it would make it worse.
Inhaled Nitric Oxide as a Therapeutic
One alternative that was tossed about early on as a potential therapeutic and subsequently addressed in numerous clinical trials, was the use of inhaled nitric oxide. The concept was that inhaled nitric oxide is quite beneficial in alleviating poor oxygenation in pulmonary hypertension (adult and pediatric). Improving local pulmonary blood flow sets up the opportunity for improved gas exchange, and thereby alleviating the damaging effects of hypoxia secondary to the COVID-19 infection.
While inhaled nitric oxide is a therapeutic boon for primary pulmonary hypertension, it failed to offer comparable benefits in clinical trials for COVID-19. WHY? Well, it was certainly predictable if you know the nuances of the pathology of COVID-19 pneumonia and how that is so different from pulmonary hypertension. One major consideration are the characteristics of the limited nitric oxide diffusion within tissues and its inherent reactivity (Limited Diffusion of Nitric Oxide in Tissues). However, in desperate times trials were pushed through by various teams (Inhaled Nitric Oxide for Managing COVID-19).
A crux of the flawed concept is that we often we forget that nitric oxide (NO) is a free radical. While it is not as reactive as some free radicals it does bear the hallmarks of free radicals in that it has limited tissue penetration and diffusion reflected in its short half-life (the time it takes for 50% of the nitric oxide to disappear via reactions with other substrates).
Early in the pandemic we knew that the lungs of infected subjects, displayed a gel like substance that formed in the lower airways. This gel created a physical barrier that limited gas exchange (oxygen for carbon dioxide) between the airways and the blood stream. This was driving the hypoxia and the perceived “heaviness” that one feels in the lungs.
What was this gel made of? Beyond leaked plasma, a major component is hyaluronic acid (Hyaluronic Acid, Lung Gel & COVID-19), a polysaccharide that is similar to mucus and used by gastropods (snails etc.) to create a platform for movement. In the lungs, hyaluronic acid is used to ease and lubricate the expansion of lungs with each breathe. Similarly, in joints the reduced friction afforded by these gels plays an important functional role. However too much of a good thing, in this case hyaluronic acid, contributes to the pathology (COVID-19 and Excessive Hyaluronic Acid ). The gel that formed in airways with COVID-19 simply formed a barrier to gas exchange. – nitric oxide and oxygen.
If inhaled nitric oxide is not reaching the blood vessels, then what is happening to it? It may connect with another free radical that is central to oxidative stress, superoxide. The result of this interaction is the generation of the very powerful oxidant, peroxynitrite. Peroxynitrite is both an oxidant and a nitrating/nitrosating substance that underlies cell damage in inflammation.
Generating Smog
On a simpler scale, nitric oxide reacts with oxygen to form the exact same, brown gases that one sees in smog, NO2 and N2O3. Indeed, my research noted that this reaction is accelerated in lipids like cell membranes at a rate of 300x (Local Generation of SMOG from Nitric Oxide ). Further, the reaction follows second order kinetics, which means that the result, NO2, is driven by the concentration of NO squared. For example, of the concentration of NO is increased 10-fold then the formation of NO2 is enhanced 100 fold (10x10). Add to that the reaction is accelerated in lipids (300x) as both NO and O2 are more soluble in lipids than water, then the potential for forming large amounts of smog is magnified enormously.
When inhaled NO was becoming popular to manage pulmonary hypertension in infants in the 1990’s, I had the opportunity to demonstrate this on stage in a Pediatric Grand Rounds shared between LSU Medical Center and Tulane Medical Center. The experiment involved saturating a large flask of water with NO, but devoid of oxygen. Then when I opened the lid of the flask exposing it to air (oxygen), a large brown cloud emerged and descended into audience. Much to their horror. The gas cloud was smog, just like you see on highways. However, Grand Rounds was not prepared for it, and they evacuated the room. My point was made – use inhaled nitric oxide carefully and consider the formation of smog in the recipient. Another consequence of this lecture was that I was asked to never do that again. Come to think of it, that was the last time I was invited to give Grand Rounds.
While I enjoyed my flirtation with WEIRD SCIENCE to academic stalwarts, I was trying to make an important point i.e., that we should never consider nitric oxide to be innocuous and devoid of complications. Indeed, some years earlier I made the breakthrough that chronic inflammation could be dramatically suppressed by inhibiting the inducible form of nitric oxide synthase (iNOS) (Chronic Inflammation is Driven by iNOS). Usually located to immune and inflammatory cells, iNOS differs from endothelial and neural NOS in that is produces NO constantly until it runs out of arginine. It is this normally dormant form of NOS that is responsible for L-arginine being classed as a semi-essential amino acid. During immune activation this otherwise dormant enzyme is activated by gene switches, and the enzyme then consumes so much arginine that supplies run out unless replenished by dietary means. It is only “essential” when there is immune activation.
During inflammation and immune activation, the oxidative stress that accompanies these conditions activates a gene switch, NF-kB, that brings iNOS out of dormancy. It also activates thousands of genes linked to immunity, inflammation and suppresses others that are responsible for repair. Activation of iNOS accompanies the cytokine storm that arises as a “All Hands On Deck” moment to combat invaders. But with that collective effort there is a lot of friendly-fire as chemical bombs are tossed around wildly.
The conclusion here is that nitric oxide, and more importantly the chemical children that it is transformed into, may not be beneficial. Indeed, it could drive and contribute to adverse outcomes as it. Hence, we are left to ponder whether it is therapeutic or culprit?
Is Nitric Oxide a Diagnostic Tool?
To address the third component of this title – is it diagnostic – let’s address a recent study where they measured the EXHALED amount of nitric oxide during COVID-19 (Exhaled NO as a Marker for Disease Severity ) . As the body produces nitric oxide it can be measured in the exhaled breath. This study examined levels of exhaled nitric oxide in COVID-19 patients divided into three categories:
· Group 1: Moderate COVID-19
· Group 2: Severe COVID-19 but without macrophage activation syndrome
· Group 3: Severe COVID-19 with macrophage activation syndrome
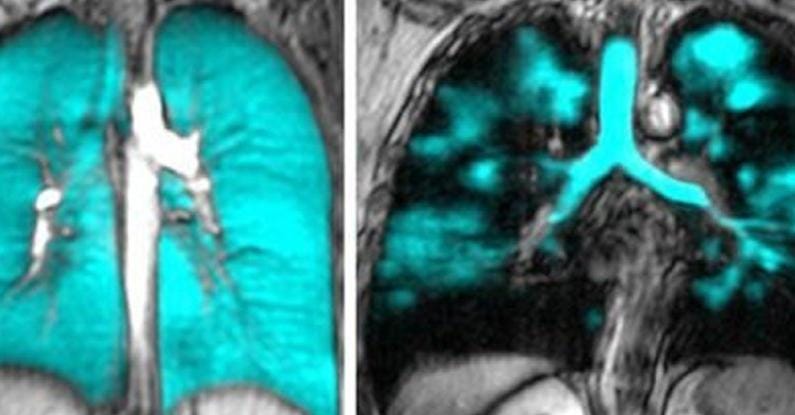
Not surprisingly the severe forms of COVID-19 had the greatest lung damage as determined by CT scans. Further, the patients with severe COVID-19 AND macrophage activation syndrome displayed the worse toll on lung morphology.
Importantly, the levels of exhaled nitric oxide were dramatically increased in both groups 2 & 3 when compared to group 1, with group 3 being the highest by far. In other words, levels of exhaled nitric oxide tracked with the severity of the disease. In this study, the authors were trying to make the point that measuring exhaled nitric oxide was a cheaper, reproducible and predictive method for assessing disease status, and should be considered as an option over the expensive CT scans.
What was not considered is that the excessive amounts of nitric oxide being formed with COVID-19 may actually be part of the burden driving the disease, and not merely markers for disease severity. Further, early concepts that nitric oxide plays an important anti-inflammatory role was challenged. Levels were greatest when the disease was at its worse suggesting that if it was playing an anti-inflammatory role, it was not very effective. Further, given that inhaled nitric oxide was not an effective therapeutic approach one must reconsider the role of nitric oxide, its enzyme sources and the ramifications of its biotransformation to other reactive nitrogen species.
It is impressive as to how the biomedical community misunderstands nitric oxide, and related events like nitration, nitrosation associated with nitrosative stress and reactive nitrogen species. Moving into the nutritional and supplement world and these misunderstandings are further compounded. In this market only endothelial production of nitric oxide is considered, or its recycling from nitrate/nitrite. The fact that nitric oxide displays a Jekyll and Hyde character (The Jekyll & HYde of Inflammation) which I proposed in 1993, is rarely entertained.
Conclusion
Finally, to answer the question posed in the title – Is nitric oxide therapeutic, diagnostic or a culprit in COVID-19 - I think we can conclude that it can be diagnostic. It may be therapeutic in very mild cases but in severe disease it is quite likely to contribute to the pathology along with the cytokine storm, excessive production of hyaluronic acid and oxidants in both acute infection and as a driver for LONG COVID and diminished recovery.